Unlike hospital and outpatient care settings, where staffing has returned to or surpassed levels seen prior to the COVID-19 pandemic, nursing home staffing continues to experience shortages. In recent years, a quarter of all nursing homes in the United States reported “critical” staff shortages amid growing demand from an aging population for long-term healthcare.
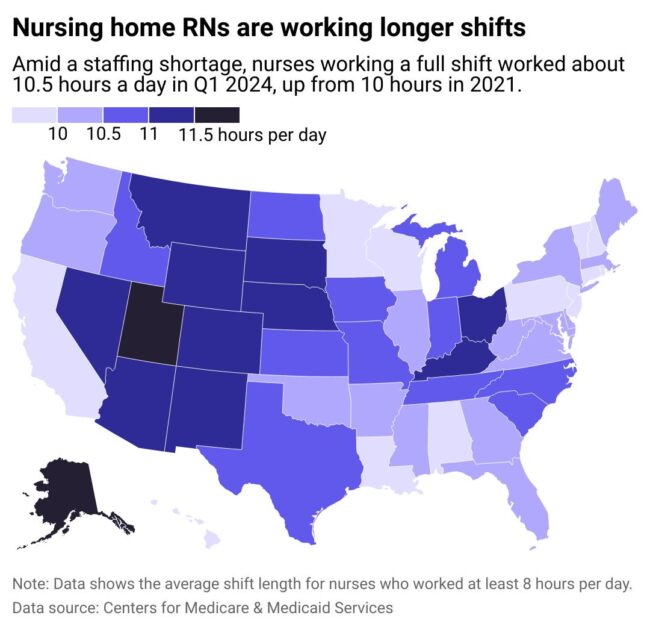
To better explore the working conditions of registered nurses (RNs) in nursing homes, Vivian Health examined payroll data compiled by the Centers for Medicare & Medicaid Services (CMS) to see where RNs in long-term care (LTC) facilities work the longest shifts. The data represents the average daily hours worked during the first three months of 2024, the latest data available.
LTC Workforce Capacity in Decline

Workforce capacity in nursing homes, already in decline before COVID-19, was further exacerbated by the pandemic, according to the 2023 “National Healthcare Quality and Disparities Report” from the Agency for Healthcare Research and Quality (AHRQ). Surges of various COVID-19 variants, including Alpha, Delta and Omicron, coincided with worsening staff shortages. That crisis has only deepened. According to the AHRQ, there were 8.4% fewer nursing and residential care workers employed in January 2023 than in January 2020.
Factors outside COVID also contribute to critical staffing shortages in LTC facilities. Burnout among nursing home care workers plays a key role in driving staffing challenges. Occupational hazards, long working shifts, exposure to violence, low salaries and high workloads have all been shown to correlate with high levels of burnout among long-term care facility nurses.
When nurses experiencing burnout opt for less stressful healthcare settings, staffing shortages grow—along with the responsibilities of remaining nursing home workers. In this vicious cycle, nearly half of new nurses report working overtime, and more than 1 in 10 nurses reported holding a second job. Newly licensed nurses, like experienced nurses, predominantly work 12-hour shifts, plus voluntary and mandatory overtime. Newly licensed nurses are also more likely to be scheduled for less desirable time slots, such as night shifts.
The combination of long shifts, holding multiple jobs and working undesirable hours can accelerate burnout for early career nurses working in nursing homes: a dangerous outcome for an already limited workforce.
RELATED: From Empathy to Exhaustion: The Hidden Toll of Compassion Fatigue and Burnout in Nursing
RNs in Alaska and Utah Work the Longest Shifts
Workplace data from CMS shows that nurses working in Alaska, Utah, Nevada, Montana and Kentucky average the longest shifts among nurses in the United States.
Alaska, where nurses work an average of 11.9-hour shifts, faces a severe nursing shortage. There are more than 1,500 reported registered nurse vacancies, a figure expected to exceed 5,000 vacancies by 2030. A new bill signed into law in July 2024 seeks to address the nursing shortage in Alaska, citing long waits for nursing licensure that deter people from pursuing a nursing career or renewing their licenses.
Utah’s nursing shortage—nurses here work 11.77 hours per shift on average—is additionally impacted by an aging nursing population. Almost 1 in 5 Utah nurses is approaching retirement age. States that have large rural areas, such as Nevada, Montana and Kentucky, also face significant challenges in part due to an uneven distribution of workers concentrated in urban and metropolitan areas.
Long work shifts and staffing shortages can lead to burnout, distress and illness among nurses—but they also tend to lower the quality of care patients receive. Nurses working longer shifts may experience increased fatigue, which can lead to errors that impact patient safety and experience. Staffing shortages have even been associated with increases in patient mortality rates.
RELATED: Nursing Shortages in 2024: A State-by-State Breakdown
New staffing requirements issued in April 2024 aim to address overburdened worker schedules and staff shortages, but most nursing homes aren’t currently equipped to meet the new standards. The American Health Care Association (AHCA) notes that 4 out of 5 nursing homes can’t meet the requirement to have nurses on staff 24/7. When all new requirements are combined, just 6% of operating long-term care facilities can currently achieve them.
With these challenges, nursing homes are limiting admissions and are concerned about closures. AHCA reports that 66% of LTC facilities are concerned that if workforce challenges persist, they may have to permanently close. This prospect could be devastating for thousands of residents, families and staff.
Download the Vivian app to find your next job in long-term care nursing today.
Feature Image Credit: Canva
Story editing by Nicole Caldwell. Additional editing by Kelly Glass. Copy editing by Tim Bruns.









