Healthcare shortages and access to healthcare have become heightened concerns across America, especially following the stress and chaos of the COVID-19 global pandemic. These struggles emphasized the significance of ensuring that all Americans have access to affordable healthcare in case of any future catastrophic health events.
Healthcare is a basic human need; however, there are citizens in many states who still struggle to access and afford this basic right despite improvements to healthcare laws. To gain a more detailed idea of where healthcare deserts exist across America, we scored each state based on their performance across six different categories related to healthcare access and affordability.
The figures analyzed in this index were obtained from six categories listed below:
- No. of available jobs per 100k people
- No. of community hospitals per 100k people
- Cost of living against the US average
- Healthcare expenditure per capita
- Healthcare insurance coverage
- Median household salary
To assess the level of healthcare access in each state, a standardized set of criteria was used to assign a score out of 100, with 100 representing the best possible healthcare access. This score provides a comprehensive overview of the current state of healthcare poverty nationwide and helps healthcare professionals (HCPs) identify areas where staffing shortages are most prevalent and where additional resources are needed.
The Worst States for Healthcare Access
Based on this research, the index revealed New York to be the most impoverished state for healthcare access, with a total score of 71.87 out of 100. This was followed by New Mexico (73.02) and New Hampshire (73.28). The states ranking as the 10 worst for healthcare access in America can be seen below.

The Best States for Healthcare Access
In contrast, Kansas received a perfect score of 100 in all categories, making it the top state in our index for healthcare access and affordability. This was followed by Nebraska (98.77) and Utah (98.51). The 10 best states for healthcare access can be seen below.

The State of Health Insurance Coverage Across the U.S.
Over the past decade, the government has implemented various initiatives aimed at enhancing healthcare coverage and services nationwide. In 2010, the Affordable Healthcare Act (ACA), also known as Obamacare, was signed into law with three primary objectives. Firstly, it aimed to make healthcare insurance more affordable and accessible to a larger number of people in the United States by reducing costs for households below the federal poverty line. Secondly, it sought to extend Medicaid coverage to those with low incomes. Thirdly, the act aimed to encourage medical innovation to help reduce the overall cost of healthcare in America.
According to the Kaiser Family Foundation (KFF), 40 states plus Washington, D.C. have now adopted the Medicaid expansion decision, ensuring more people can access fairly priced insurance. Only 10 states, including Texas, Florida, Kansas and Georgia, have not adopted the expansion.
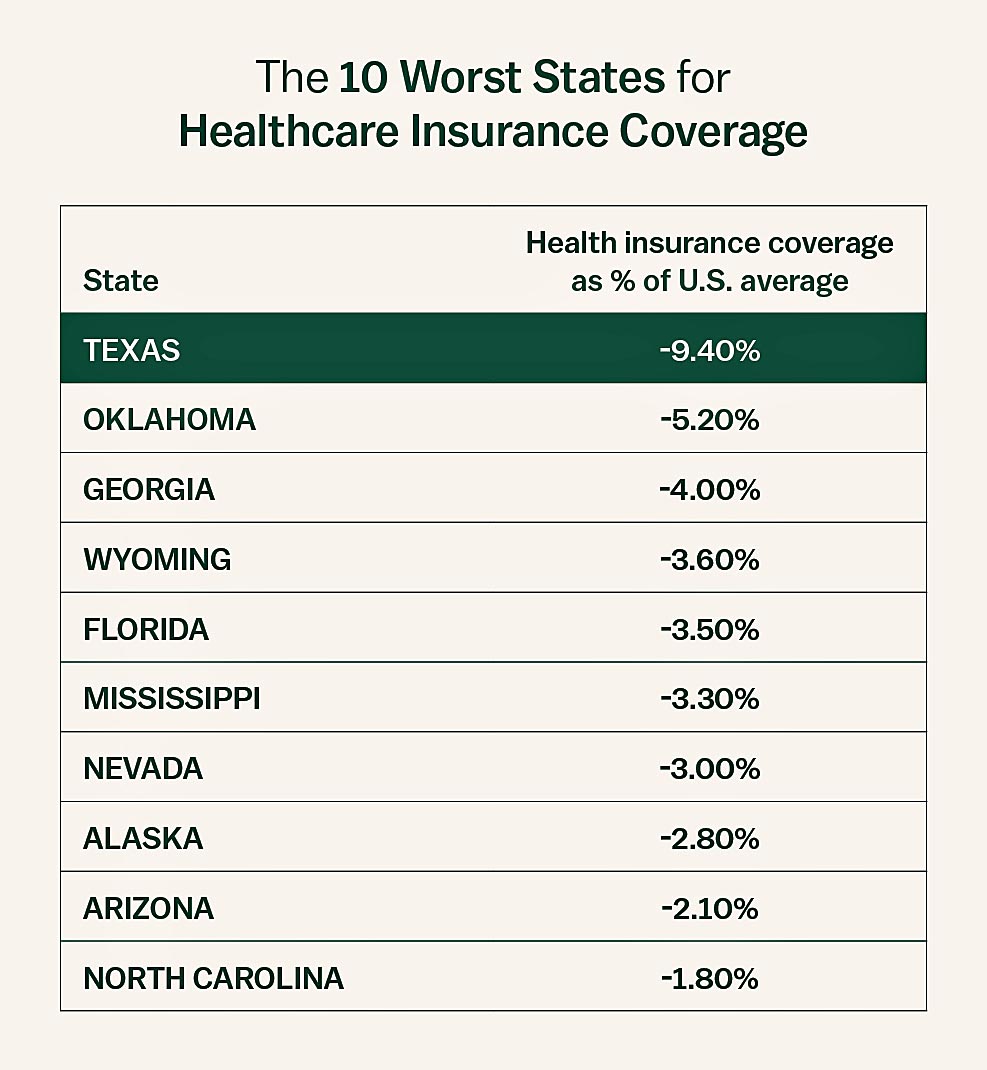
The Worst States for Healthcare Insurance Coverage
Our research on the Vivian Health Index highlighted that certain states still have inadequate health insurance coverage, which puts a significant number of people at risk.
According to our index, Texas has the lowest health insurance coverage rate compared to the rest of the United States, with a 9.4% difference. Interestingly, many of the states with the lowest rankings in our index have not yet decided to adopt the Medicaid expansion, including Wyoming, Georgia, Florida and Texas. This suggests a correlation between these states’ decisions and their low health insurance coverage rates.
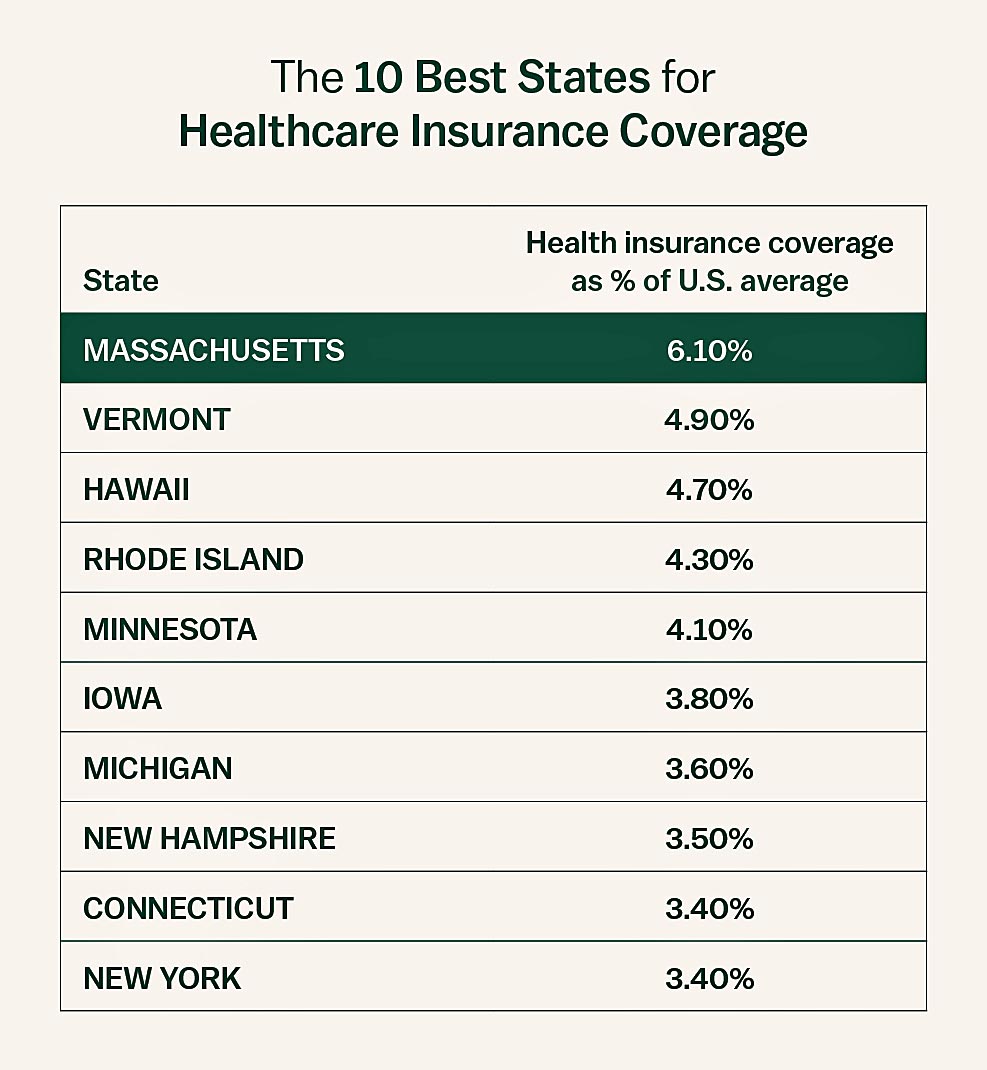
The Best States for Health Insurance Coverage
Although there are challenges to overcome, our analysis of data has shown that certain states have higher rates of insurance coverage compared to the national average. Massachusetts ranked as the top state in our index, with 6.1% greater health insurance coverage compared to the U.S. average. It is worth noting that all of the top 10 states have implemented Medicaid expansion programs, which aim to provide healthcare coverage to more individuals.
Why Are Some Americans Uninsured?
Low income is the main cause of uninsured Americans, per KFF population data. According to this study, the majority of individuals without health insurance come from low-income households that have at least one employed member. Due to the lack of public health coverage in certain areas, adults are more prone to being uninsured compared to children.
Although policies such as the ACA and Medicaid expansion were implemented to make coverage more affordable, there are still many people who remain uninsured due to the high cost of insurance being a primary barrier. For example, in 2021, 64% of uninsured adults reported in a KFF study that they were uninsured due to the high cost of premiums.
Many individuals lack job-provided insurance, and certain low-income adults in non-Medicaid expanding states are still ineligible for coverage that is based on financial assistance.
Why Health Equity Is Important to Healthcare Workers
The lack of healthcare services in certain areas is a major concern for the public and can also impact HCPs. These problems can increase the workload of HCPs, limit career growth opportunities and potentially reduce income potential.
Social Support for the Disadvantaged
Nurses, allied health professionals and other healthcare workers should lead the charge in advocating for policies that address restricted access to healthcare. These HCPs often enter the field with the goal of serving the social, emotional and physical needs of marginalized populations, which healthcare equity initiatives aim to address.
According to the National Center for Health Statistics, individuals who are socially and economically disadvantaged have a higher likelihood of experiencing poorer health, lack of access to quality healthcare services and premature death compared to those who are socially and economically advantaged. As a result, improving access to healthcare for all is crucial.
Understanding the Healthcare Employment Landscape
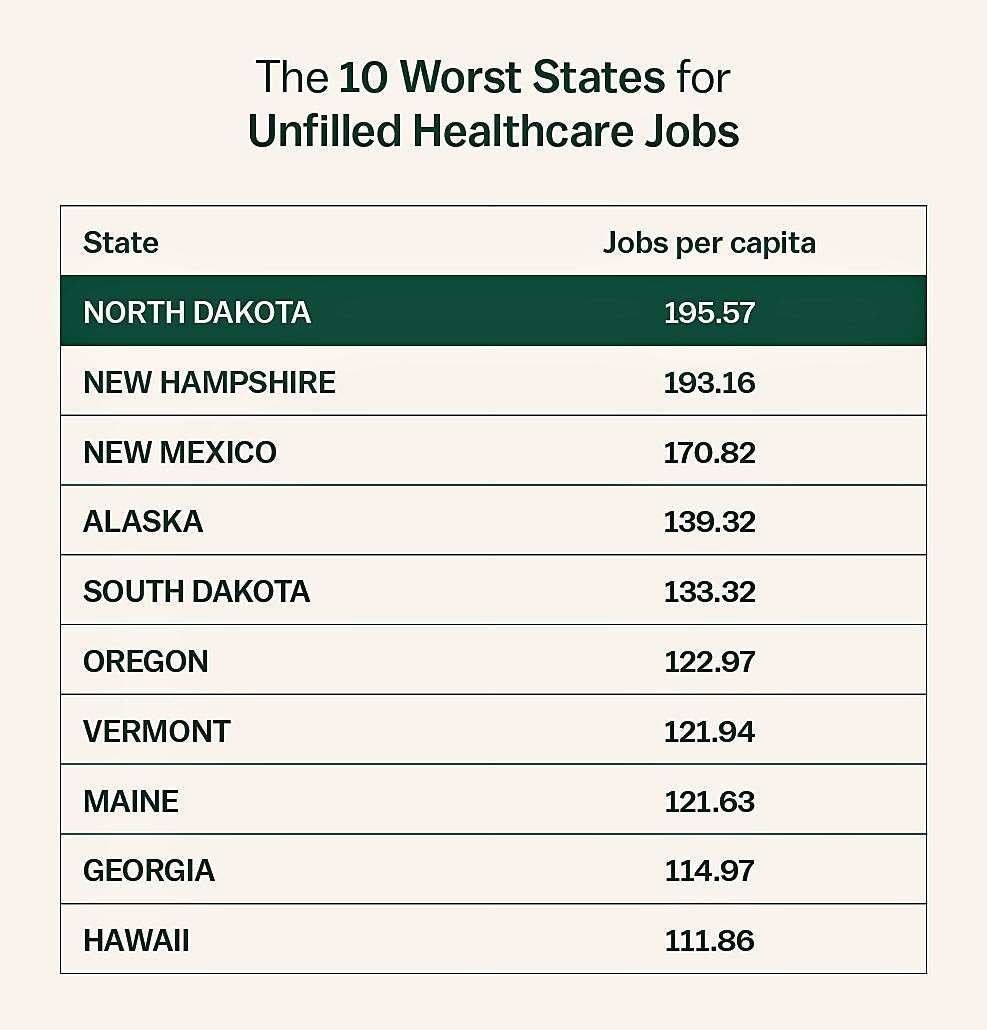
Within our index, one of the main categories states were ranked on was the number of unfilled healthcare jobs per capita. By analyzing vacant jobs, we identified areas where many healthcare and nurse shortages exist and areas that are underserved. This analysis helps applicants make more informed decisions when searching for their next staff or travel assignment.
At the time of writing, North Dakota had the most unfilled healthcare positions per capita at 196 jobs per 100k of the population. This corresponds to our 2023 index: The Best States for Travel Nurses to Work, which identified the Dakotas as the best state for travel nurses to work. However, the abundance of vacancies also indicates a decrease in public access to healthcare professionals in this area. The following list displays the top 10 states with the most unfilled positions.
How Medical Professionals Can Improve Health Equity
Improving poverty levels and addressing disparities in America is not the primary responsibility of our key medical workers. However, due to their crucial role in enhancing health across the nation, they possess the ability to steer this change in the right direction. According to the National Academies of Science Journal, nurses can play a significant part in reshaping the health equity landscape in the upcoming decade by exploring new settings and methods and advocating for policy changes.
The journal highlights that certain nurses are already engaged in roles and settings that promote health equity and are actively educating and advocating for it through their professional organizations. Nevertheless, with broader involvement from medical professionals, every nurse can contribute to advancing health equity on a national level.
Continue to explore more U.S. data and employment trends in our 2023 Index: The Best States for Travel Nurses to Work.
© Vivian Health 2023









